Is Sex Off the Table, or Are Certain Sexual Acts a Bad Idea?
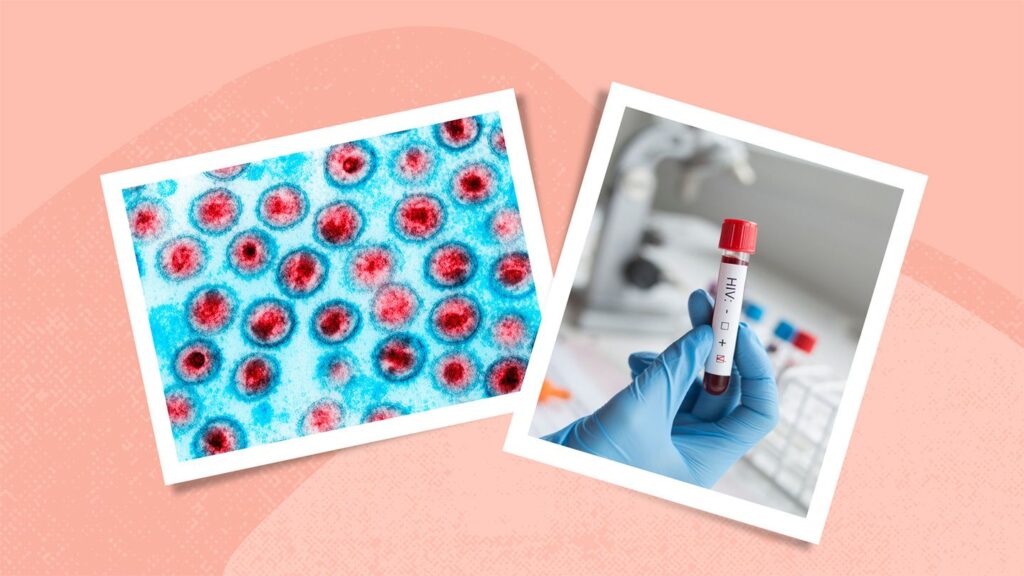
Sex is definitely not off the table if you’re dating someone who has HIV, although it’s a good idea to be cautious until you know that your partner’s treatment is effectively suppressing the virus. “We want to see their viral load persistently undetectable for six months before we say they’re not at risk for transmitting the virus,” says Michael Wohlfeiler, MD, chief medical officer of the AIDS Healthcare Foundation.
Until you know that your partner’s treatment is working as it should, you can take certain steps to ensure that you are protected, such as taking PrEP or using condoms. Additionally, different types of sex have different risks for HIV transmission. It’s important to use condoms or take PrEP if you’re having anal or vaginal intercourse, says Dr. Wohlfeiler. There is little to no risk of transmitting HIV through oral sex, including oral-anal contact, although theoretically it could be spread if semen comes in contact with an open mouth sore or bleeding gums. For this reason, Dr. Gandhi says, “use PrEP if there are any mouth sores that could increase the chance of transmissibility,” or use condoms for oral sex until you know that your partner’s treatment is working.
Is There Any Risk From Kissing My Partner?
Is It Safe to Share Food, Toilets, or Toothbrushes?
What Does It Mean if My Partner’s Viral Load Is Undetectable?
If your partner stays on top of their treatment schedule and HIV in their blood remains undetectable in lab tests, they cannot transmit HIV to you or anyone else.
If someone with an undetectable viral load keeps taking their treatment as prescribed, they can expect to remain undetectable indefinitely, Wohlfeiler emphasizes.
What Role Do Condoms Play in HIV Prevention?
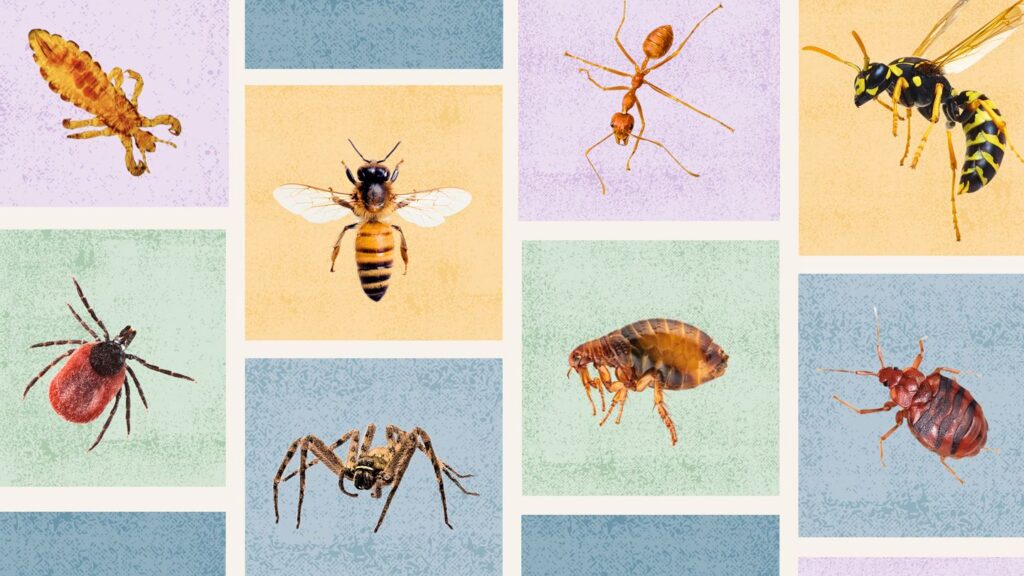
If your relationship isn’t monogamous, “I would recommend condoms to protect your partner, especially if they don’t know you’re nonmonogamous, because of the STD risk (aside from HIV),” says Gandhi, noting that while STDs are treatable, “they can have harmful effects,” including significant discomfort. And of course, using condoms helps protect you from getting HIV from other sexual partners.
Should I Take Medication to Help Prevent HIV?
“If someone is not undetectable or for some reason can’t take their HIV medications every day, I would definitely want the negative individual to be on PrEP,” says Gandhi. “Treatment as prevention relies on people taking their medications and staying undetectable.”
Going on PrEP is also a good idea if your relationship isn’t monogamous and you’re regularly having sex with different partners, says Wohlfeiler. “If you’re going to have occasional encounters outside the relationship,” he notes, “condoms are just as effective at preventing HIV and also have the advantage of protecting you from other STDs.”
Should I Get Tested for HIV Regularly?
For someone who has an HIV-positive partner, getting tested regularly is “just good preventive healthcare,” Gandhi notes, even though your risk of getting HIV from your partner is essentially zero if their viral load remains undetectable.
What Can I Do to Support My Partner?
You can help your partner manage HIV in plenty of ways.
Wohlfeiler agrees that it’s essential to help your partner remember to take their medication consistently — for their health and for yours. “We recommend everything from reminders on their cell phone to putting it in the kitchen next to the cereal or on the night table, so they get these cues to take it,” he says. “I think the negative partner often has a fairly active role in saying, ‘Did you take your medicine?’”
The Takeaway
Learning that your partner has HIV can be overwhelming, but you can reduce your risk of getting HIV to essentially zero with effective prevention methods such as ART and PrEP. Regular HIV testing is recommended. You can also support your partner by encouraging them to stay on top of their treatment regimen and follow up regularly with their doctor to ensure their HIV levels remain undetectable.